Medicaid work requirements pose huge challenges for states
Published in Political News
WASHINGTON — Congress is on the verge of passing legislation that would require millions of Medicaid beneficiaries across the nation to prove they are working to receive benefits, posing a massive challenge for states that would be required to act quickly with limited resources.
The requirements, a prominent feature of Republicans’ budget reconciliation bill that passed the House last month, would apply to millions of people who are eligible for Medicaid under the 2010 health care law’s expansion: mainly low-income adults who don’t earn enough money to buy their own insurance or get it through their jobs. The Senate Finance Committee included the same requirements in its version of the proposal released Monday evening.
State Medicaid directors, including those representing red states, have privately told drafters of the legislation that a Dec. 31, 2026, effective date in both versions would be too soon to implement work requirement programs that actually aim to help people rather than kick them off for noncompliance.
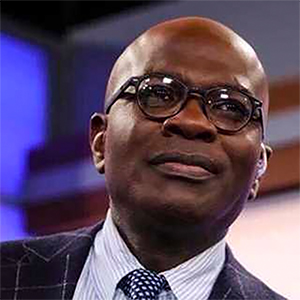
“Every Republican state, every red state I’ve talked to has had a very similar approach: We like the idea but also want to implement it in such a way that it’s going to have a meaningful, positive influence on the people we serve,” said Matt Salo, founder and CEO of Salo Health Strategies and former director of the National Association of Medicaid Directors. “I think 2026 implementation would only be possible with an infrastructure investment that doesn’t currently exist. … What [states] don’t want to do is create a policy where people lose coverage because of paperwork or they didn’t fill out a form correctly.”
But Salo warns that is what will happen if states must implement work requirements by the end of next year.
Those warnings haven’t deterred congressional Republicans who are eager to reduce Medicaid spending.
“If we can’t pull it off by next year, what’s wrong with us?” said Republican Sen. Jim Justice, who, until earlier this year, was governor of West Virginia.
Asked whether his state’s Medicaid systems are able to verify compliance with work requirements, he responded, “We’ll screw it up some. I mean, that’s all there is to it, for sure. But we don’t need four years or three years to try to figure this out on what to do.”
Sen. Josh Hawley, R-Mo., has fought against other cuts to Medicaid. But when asked whether he was concerned about people inadvertently losing coverage because of paperwork or systems issues with the work program, he replied, “I’m for work requirements.”
Under the work provisions, before enrolling in the program, “healthy” adults between the ages of 19 and 64 years must prove they had worked at least 80 hours in the month prior to enrollment. They must also meet the requirements for at least one month between eligibility checks that states must conduct every six months.
Being enrolled in job training or in an educational program at least half time would also count. Those seeking Medicaid coverage could prove they are exempt for other reasons, including being “medically frail” or homeless, having a substance use disorder, and being a parent or caretaker of someone with disabilities.
The requirements would save $344 billion over 10 years, according to the Congressional Budget Office, and result in 5.2 million fewer people enrolled in Medicaid by 2034.
Tighter deadline
Implementing the requirements would be a huge undertaking for states. They would be responsible not just for checking whether beneficiaries are working or in school but also determining whether people qualify for the multitude of exemptions, as well as informing beneficiaries of changes and designing programs to connect people to educational or employment resources.
All of those challenges are compounded by the decision of House Republican leadership to speed up the implementation date from the original language by three years to the end of 2026. That was intended to generate more Medicaid savings in the House bill.
“Eighteen months is not a realistic turnaround time given everything that’s going on in the world,” Salo said. “Can you implement something quickly? Yes. Will it be effective, will it be humane, will it be member-focused and person-centric? Probably not.”
Neither the Senate nor the House version provides funding for states to hire people or build out these programs. They do provide $100 million total in grants to states to upgrade their systems, which directors have said is not nearly enough.
For example, Georgia, which was granted a waiver by the Centers for Medicare & Medicaid Services to implement a similar version of Medicaid work requirements, spent more than $50 million on administration and upgrading its Medicaid systems.
Experts have always warned that work requirements could result in coverage losses, including those who are employed but get lost in a bureaucratic maze of government systems. Previous CBO scores have estimated that Medicaid work requirements would not increase employment but would increase coverage losses. But the speedy time frame for implementation could compound those issues.
The bill says that states should, when possible, use data to automatically determine whether someone is already meeting the requirement or would be exempt. Drafters said they learned lessons from a failed attempt in Arkansas to implement Medicaid work requirements in 2018 in which 18,000 people, many who were working or would have been exempt, lost coverage.
But for some states, such data doesn’t exist. They have data to verify Medicaid’s income requirements but don’t know how many hours people are working. Data from the Internal Revenue Service can be made available to states, but it’s challenging to access and can be as much as 2 years old, according to the Medicaid and CHIP Payment and Access Commission. That renders it of little use for verifying compliance with a current work requirement.
Getting information about beneficiaries’ incomes or employment can be challenging for people with unstable incomes, including those who are self-employed or seasonally employed or who frequently change jobs, according to MEDPAC.
“That’s a very important way states can mitigate coverage losses, but states’ capacity to use these data systems varies very widely, which we saw during the unwinding of the continuous coverage requirement” after the COVID-19 public health emergency, said Michael Karpman, a principal research associate in the Health Policy Division at the Urban Institute.
“And those databases don’t include all workers, especially people who are self-employed or involved in gig work or have other nonstandard work arrangements, which include a lot of people working at low wages,” he said.
States also have no way to track where and how often people are volunteering, an alternative to working that fulfills the requirements. Information on such exceptions may exist only in limited capacity.
The reconciliation package includes exemptions for vulnerable people the system already struggles to keep engaged with the health care system, including those who are homeless or experiencing substance use disorders — sometimes at the same time.
Some states have more information on this than others, but the systems at various agencies aren’t integrated. Data sets may contradict each other, such as those tracking exemptions from work requirements for people receiving food assistance.
Outreach pitfalls
Without significant upgrades to systems that can provide a clearer picture into the lives and circumstances of Medicaid beneficiaries, states will have to get that information directly from individuals. That creates its own challenges.
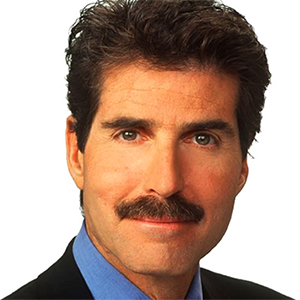
“We just went through this last year,” said Craig Kennedy, CEO of Medicaid Health Plans of America, referring to the process that states undertook after the pandemic to review and remove people from their Medicaid rolls who were no longer eligible. During that health emergency, states were prevented from removing people from Medicaid to ensure they retained access to health care.
“Most people lost their Medicaid coverage for procedural reasons, not eligibility reasons. I think that’s an important aspect to remember as we go into these new mandates,” Kennedy said.
That may be because states were required to confirm eligibility using existing data, although many did not. In North Carolina, for example, 99% of renewal decisions utilized existing data, compared with 12% in Pennsylvania as of October 2023.
Some of those removed eventually signed up for Medicaid again or got other insurance. Others remained uninsured. States cited limited resources and competing priorities in conducting automatic renewals, including state budget constraints.
When states can’t verify eligibility using data, they must reach out to beneficiaries. That introduces potential complications. Letters get lost in the mail, and beneficiaries may be confused about what is required of them.
“People are going to lose coverage not because they’re not looking for work or engaged in the community but because they failed procedural hurdles to keep coverage,” Kennedy said.
©2025 CQ-Roll Call, Inc., All Rights Reserved. Visit cqrollcall.com. Distributed by Tribune Content Agency, LLC.



















































Comments